Children’s Vision
Assessing children’s vision can be challenging. It is not possible to ask questions as we would with adults and their responses can be misleading.
Children’s eyes can be examined during their first year of life. Many people are under the impression a child needs to recognise the alphabet in order to be tested. However, this is not initially required.
It is important to understand that seeing the lowest line on the letter chart does not necessarily mean that visual function is working efficiently.
A child comprehends what they see if they can see it clearly and comfortably. There are three factors which determine if a child’s eye is operating efficiently:
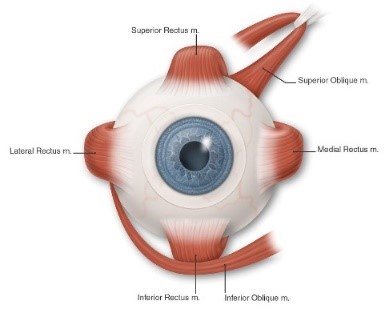
1- The external 6 muscles of the eyes must be aligned and work in synchrony with each other. These 6 muscles are known as the extra ocular muscles and are responsible to move the eyes around and point to a target.
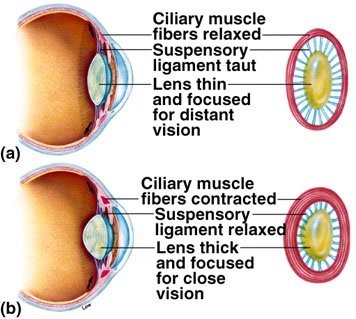
2- The internal muscles of the eye are known as the ciliary muscles. These muscles are attached to the lens in the eye. They tense up and relax to zoom the lens in and out of focus to clear targets.
3- The anatomy of the eye needs to be clear of any pathology to allow the light to focus at the back of the eye (retina) in order to be processed.
If any of the above factors are compromised, then the visual system becomes compromised. At such a young age, the brain begins to rewire and remodel how it operates to manipulate the function of the eye in attempt to achieve some form of vision.
Squint

A squint (also called strabismus, or a turn in the eye) refers to any ocular misalignment. This happens when both eyes are not looking in the same directions and are not focussing on the same target. The deviating eye can either turn inwards (esotropia), outwards (exotropia), upwards (hypertropia) or downwards (hypotropia). A squint can be intermittently occurring or constant. A squint can either be in 1 eye or alternate between the eyes.
Management of a squint commonly involves glasses and patching, but exercises (Orthoptic therapy) or surgery are sometimes required. The most important factor for a good outcome is early detection and most preferably before the age of 6-8years of age.
At Daling St Optometrix, Hayssam has all the postgraduate knowledge and experience to detect and treat children’s eye turns.
Amblyopia
Amblyopia (or lazy vision) occurs when the brain does not receive a clear image from one eye. The image could be blurred or doubled and so the brain chooses to ignore the image and not use that eye giving rise to its “lazy” nature.
It is very important to note that it is not the eye that sees! It is actually the brain that sees. The eye is a mere tool to focus and deliver the image to the brain. During the first decade of life, the visual part of the brain (visual cortex) develops and models how we see. This is otherwise known as neuroplasticity. If the eye is not delivering a clear signal to the brain, that part of the brain becomes under developed and supresses the image from the eye.
If amblyopia is detected early, before the age of 10, it is possible to train the brain to see and model correctly.
Blurred Vision
Refractive error is a focusing problem whereby someone is long-sighted, short-sighted or astigmatic. It is caused by the length of the eye being too long (myopia), short (hypermetropia), or slightly irregular in shape (astigmatism). It is corrected by wearing glasses.
If left untreated during the first decade in life, it could lead to amblyopia and/or a turned eye.

Colour Vision
Colour vision deficiency may be inherited (and present since birth) or acquired later in life as a result of a disease of the eye. If inherited, it is usually detected during the child’s first eye examination using an Ishihara test plate. Colour deficiencies are usually more common in males than females because it affects the X chromosome. That is, females have two X chromosomes and males have one X and one Y chromosome. Hence, males will usually acquire the affected X chromosome where as females will carry the affected X chromosome.
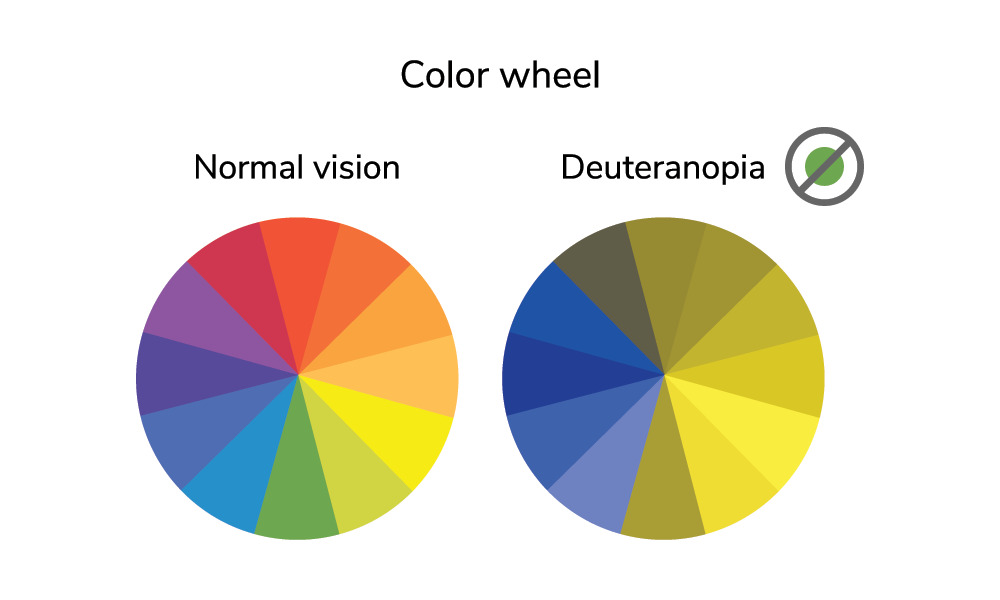
We have 3 colour cells in our eyes. One detects red. One detects green and one detects yellow/blue. If one of these cells is absent or affected, it results in a colour vision deficiency. Patients who have a colour deficiency do not see black and white. They usually have a problem with identifying different colours. For example, if a patient has a red green colour deficiency, this is called deutranopia. Their perception of colour is illustrated below.
Swollen Optic Nerve Head
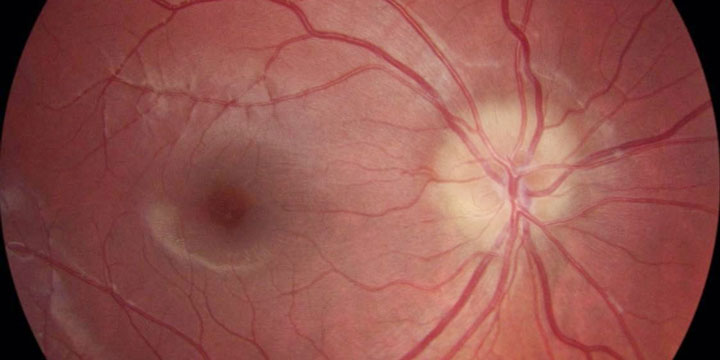
Swelling at the optic nerve head may be a co-incidental finding with benign nature. However, if detected, it is always treated seriously in case there is a neurological or auto immune condition.
If children complain of headaches, dizziness, loss in vision or blurred vision, retinal photography is one of the best ways to detect this and prompt referral for further investigation.
Chalazion (Cyst of the eyelid)

Otherwise known as a stye, a chalazion is a blockage of one of the Meibomian glands (oil glands in the eyelids). It can appear as a lump on or near the eyelid margin. Sometimes a secondary infection can develop and antibiotics are required.
Most patients presenting to a medical physician are prescribed an antibacterial ointment such as Chloramphenicol. Whilst this is an excellent prophylactic approach to a Chalazion, it does not entirely treat the blockage of the oil gland.
It is best to diagnose a chalazion early and treat it with heat packs and lid cleaning wipes. If left alone for some time, the cyst may harden or become infected and require an operation to be drained and removed.
Watery Eye

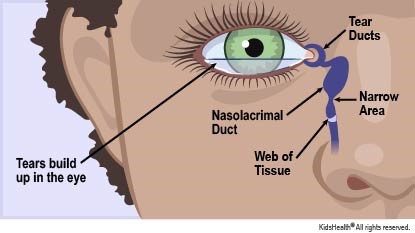
Up to 20% of the newborn population have watery, sticky eyes. Normally, the eye produces tears to wash and lubricate the ocular surface and these flow down the tear duct and into the nose. When a baby’s eyes are excessively watery and/or sticky it is usually due to a delay in opening of the tear duct.
It is estimated that 80% of babies affected will spontaneously improve once the tear duct finishes developing within the first 6-12 months of life. If it fails to spontaneously improve, a probing of the tear duct under general anaesthetic by a qualified Ophthalmologist is usually successful in curing this problem.
If the watery eye is associated with a redness or excess mucous, it is important to be assessed incase antibacterial eye drops are required.
Conjunctivitis
Conjunctivitis, also known as “pink eye”, is a swelling and/or an infection of the conjunctiva (clear membrane covering the eye ball). It is a very common problem in children. Large outbreaks of conjunctivitis are often seen in childcare or pre-school settings. The most common causes of childhood conjunctivitis are:
- Bacteria
- Viruses, including the herpes virus
- Allergies
If the condition is caused by an infection, it is important to know that the infection can spread from one eye to the other by touching the affected eye or fluid from the eye. The infection can also spread to other people. Fluid from the eye is still contagious for 24 to 48 hours after starting treatment.
It is important to differentiate a pink eye from an emergency red eye to achieve a quick and efficient recovery.